Diabetic neuropathy is one of the most common and debilitating complications of diabetes. Its causes and mechanisms are complex, involving a range of genetic, metabolic, and oxidative stress factors that damage the peripheral nerves. Here, we’ll explore the main contributors to this condition and how these factors interact.

Key Causes of Diabetic Neuropathy
Research indicates that diabetic neuropathy is a multifactorial condition with the following contributing factors:
- Genetic Predisposition Genetic factors may make some individuals more vulnerable to nerve damage from elevated blood glucose. Variations in certain genes are linked to a higher risk of neuropathy in diabetic patients.
- Ischemia and Hypoxia High blood sugar levels impair blood flow to nerves, leading to ischemia (reduced blood flow) and hypoxia (lack of oxygen). This restriction starves the nerves of essential nutrients and oxygen, resulting in nerve degeneration over time.
- Oxidative Stress Oxidative stress occurs when an excess of free radicals overwhelms the body’s antioxidant defenses. In diabetes, high glucose levels accelerate the production of free radicals, damaging nerve cells. This process contributes to chronic inflammation and plays a major role in the progression of diabetic neuropathy.
- Polyol Pathway Overactivity In diabetic patients, excess glucose is converted to sorbitol through the polyol pathway. Sorbitol accumulates in nerve cells, leading to osmotic stress, swelling, and damage to the nerve fibers.
- Advanced Glycation End Products (AGEs) Chronic high blood sugar leads to the formation of advanced glycation end products (AGEs), which bind to receptors on nerve cells (RAGE) and activate nuclear factor NF-KB. This activation results in inflammation and oxidative damage, impairing nerve function.
- Protein Kinase C Activation High glucose also activates protein kinase C (PKC), which affects blood flow regulation and nerve cell survival. PKC activation disrupts blood supply to the nerves and exacerbates oxidative stress, contributing to nerve damage.
- Essential Fatty Acid Metabolism Diabetic patients often experience disturbances in essential fatty acid metabolism, which can impact nerve structure and function. Fatty acids are crucial for nerve health, and imbalances can weaken nerve cell membranes, making them more susceptible to damage.
- Deficiency of Neurotrophic Factors Growth factors like nerve growth factor (NGF) and insulin-like growth factor 1 (IGF-1) are essential for nerve maintenance and repair. In diabetes, these growth factors are often deficient, leading to reduced support for nerve regeneration and resilience.
The Complex Pathogenesis of Diabetic Neuropathy
The development of diabetic neuropathy involves multiple interconnected mechanisms. High blood glucose initiates a cascade that affects nerve blood flow, nerve cell metabolism, and inflammatory responses. Here is a simplified view of the pathogenesis:
- Reduced Blood Flow: High glucose levels cause blood vessels to constrict, reducing blood flow to the nerves. This limits the oxygen supply, setting off ischemia and oxidative damage.
- Activation of Harmful Pathways: The polyol pathway, AGE formation, and PKC activation further contribute to nerve stress. Increased blood viscosity due to high glucose levels slows blood flow, leading to increased adhesion of inflammatory cells to the blood vessels, further blocking blood and oxygen supply.
- Inflammation and Oxidative Damage: Oxidative stress and the accumulation of AGEs induce chronic inflammation, damaging the nerves and creating a feedback loop that accelerates nerve degeneration.
- Deficiency of Neurotrophic Support: A lack of growth factors essential for nerve repair weakens the nerve’s resilience, leaving it vulnerable to damage.
- Apoptosis of Nerve Cells: High levels of oxidative stress and inflammation result in apoptosis (cell death) of nerve cells, which leads to permanent nerve loss if left unchecked.
This interplay of mechanisms illustrates the multifaceted nature of diabetic neuropathy, with each factor amplifying the effects of others. As a result, diabetic neuropathy can be difficult to reverse, making early detection and management crucial.
MAIKONG.LTD’s Solutions for Diabetic Neuropathy
MAIKONG.LTD specializes in developing advanced diagnostic and therapeutic devices designed to support diabetes management. Key products include:
- Biothesiometer VPT: Measures nerve sensitivity and vibration perception, helping to detect neuropathy early.
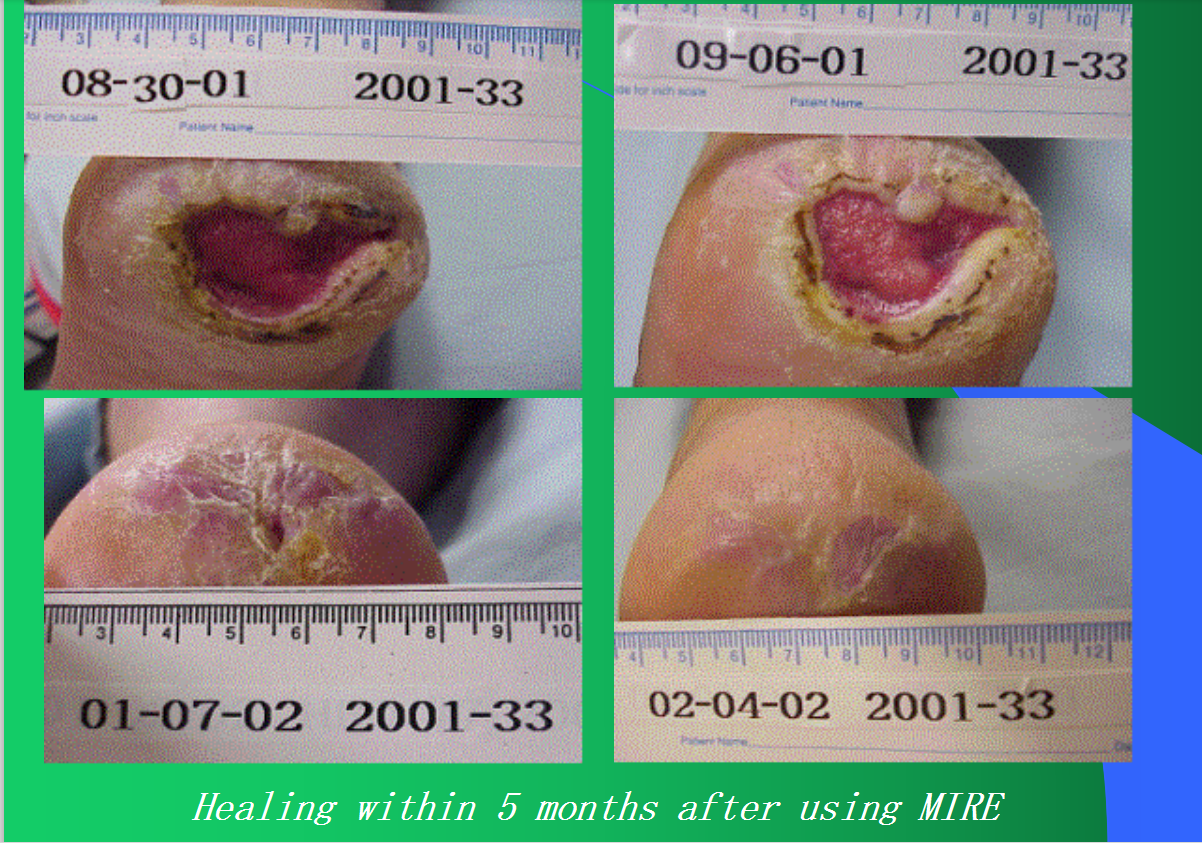
- Peripheral Neuropathy Therapy System: Delivers targeted therapy to improve blood flow and reduce neuropathy symptoms.
- OEM/ODM Customization: MAIKONG.LTD offers customization options for branding, appearance, and packaging to meet the needs of various healthcare providers globally.
FAQs
1. What is the main cause of diabetic neuropathy?
The primary cause is prolonged high blood glucose, which damages the nerves through mechanisms like oxidative stress, blood flow impairment, and inflammation.
2. Can diabetic neuropathy be reversed?
While difficult to reverse fully, early detection and blood sugar control can slow its progression and alleviate symptoms.
3. What diagnostic tools does MAIKONG.LTD provide?
MAIKONG.LTD offers devices like the Biothesiometer VPT for detecting sensory loss, and therapeutic systems to support nerve health.
4. How can oxidative stress be reduced in diabetic patients?
Controlling blood glucose, taking antioxidant-rich foods or supplements, and regular monitoring can help reduce oxidative stress.
5. What role does blood flow play in diabetic neuropathy?
Reduced blood flow due to high blood glucose deprives nerves of oxygen and nutrients, leading to nerve damage over time.
For more information about advanced diagnostic tools and management solutions, contact MAIKONG.LTD to learn how our devices can help in early detection and effective management of diabetic neuropathy.